|
Formula
|
Fluid
in First 24 Hours
|
Crystalloid in 2nd 24-Hours
|
Colloid in 2nd 24-Hours
|
|
Brooke (Yowler, 2000)
|
RL at 1.5 mL/kg per percentage burn, colloid at 0.5 mL/kg
per percentage burn,
- add 2000 mL D5W
|
50% of first 24-hour volume -
add
2000 mL D5W
|
50% of first 24-hour volume
|
|
Modified Brooke
|
RL at 2 mL/kg per percentage burn
|
|
|
|
Evans (Yowler, 2000)
|
NS at 1 mL/kg per percentage
burn, 2000 mL D5W*, and colloid at 1 mL/kg per percentage burn
|
50% of first 24-hour volume and add 2000 mL D5W
|
50% of first 24-hour volume
|
|
Monafo hypertonic
Demling |
250 mEq/L saline titrated to urine output at 30 mL/h,
dextran 40 in NS at 2 mL/kg/h for 8 hours, RL titrated to urine output at 30
mL/h, and fresh frozen plasma 0.5 mL/h for 18 hours beginning 8 hours post
burn
|
One-third NS titrated to urine output
|
|
|
Metro Health
(Cleveland) |
RL solution with 50 mEq sodium bicarbonate per liter at 4
mL/kg per percentage burn
|
Half NS titrated to urine output
|
1 U fresh frozen plasma for each liter of half NS used
and add
D5W as needed for
hypoglycemia
|
|
Slater (Yowler, 2000)
|
RL at 2 L/24 h and
add fresh frozen plasma at 75 mL/kg/24
h
|
|
|
Wednesday, April 16, 2014
Burns treatment, resuscitation in burns, formula, managing burn patients…..
Doc, you described the fluid requirement in the first 24 hrs, what
happens in the next 24 hrs? How do we calculate the fluid requirements for
that?
One more question- you gave a few formulas for the burn calculation,
could you outline some more?
Surya, N Delhi, India
The formula for fluid resuscitation
help to calculate the fluid requirements for the first 24 hours. It is during
this period that the critical fluid displacements and loss occur. Loss of body
fluids from the burn surface area as well as the leaking of intravascular
fluids into the extracellular spaces account for the fluid loss that occur in
burn patients. However the body regains its capacity to maintain its intravascular
volume by avoiding the leaking of plasma proteins and in fact by the 2nd
24 hours after the burn, the fluids from the extra vascular spaces start
getting reabsorbed. Therefore at this stage it is not necessary to administer a
lot of fluids as we do in the first 24 hours. During the second 24 hours the
fluids are calculated from the normal daily requirements as any surgical
patient and additional fluids are given to maintain the clinical parameters
like the pulse, blood pressure and urine output (half ml/kg/hr in adults and
one ml/kg/hr in children) as outlined in a previous post.
Some formulas advice cutting down the
fluids to be administered in the 2nd 24 hours to half that of the
first 24 hours. This again is a guideline and one must not forget that the
resuscitation process is a continuous process and no sudden changes must be
attempted in fluid administered which must be very gradually reduced depending
on the clinical parameters and patient response unless the patient is in shock
or with volume overload.
The parkland formula has been
described before in detail. Some of the other resuscitation formulas which were
not mentioned in our previous articles are outlined below:
Resuscitation Formulas in burn patients
*D5W is
dextrose 5% with water
(An original initiative in burn care and education from asktheburnsurgeon++)+
Saturday, April 12, 2014
Burns in children……
Fluid
resuscitation in pediatric population
Doc, are burns in small children more
serious than in adults? Also please tell how does the resuscitation of burn
patients differ in adults and in children?
Milnarnake p,
Sri Lanka.
Management of burns in children differs
significantly from that in adults. This is because the fluid loss in burns
depends on the total body surface area that is burnt and the calculation of the
body surface area is different in adults and children. When compared to adults
it has been found that children have larger head and smaller thighs. Thus while
in adults the head is taken as 9 percent in a newborn or infant it is 20
percent TBSA. Similarly the lower limbs account for 18 percent in adults, however
in an infant it accounts for only 13 percent TBSA, since the infant has a
smaller limb size compared to adults in proportion to the head. Again the upper
limbs account for 9 percent each in adults, but in children this is only eight
percent. In adults the front and back of the body or trunk account for 18 percent
but in infants it is 20 percent.
Thus in an infant
Head – 20
Both upper limbs – 8x2=16
Both lower limbs 13x2=26
Back of trunk -18-20
Front of trunk – 18-20
This all approximates to about 100
percent
To get the most accurate calculation
in children the Lund and Browder chart should be used.
Urine output/hour which is one of the
most important clinical parameter in monitoring burn patients should be 1 ml/hr
in children as compared to adults (0.5 ml/hr). Children who are over 50 kg
should be managed as adults for calculating the fluid requirement. Minor burns
in children (less than 10% usually do not need any fluid resuscitation as the
body can handle this fluid loss. However children with over 10% burns need
fluid resuscitation as compared to adults over 15%. The requirements in
children are higher and most centers add maintenance fluids to their
resuscitation formula.
It is interesting to note that if the
parkland formula as used in adults
i.e. 4x %TBSA x body weight is used in children,
the fluid calculated will be inadequate and therefore a modified parkland
formula is used in children-
3 x %TBSA x body wt + daily maintenance
fluid requirements
How do we calculate the daily fluid requirement in a child? Here’s a
simple method:
First 10 kg- 100ml/kg
Second 10 kg- 50ml/kg
Rest of kgs- 20 ml/hr
This is the total maintenance fluid requirement
for 24 hrs and this is divided by 24 or 25 to get the per hour calculation
Imagine a child with 25 kg- what is
the maintenance fluid requirement for 24 hrs?
First 10 kg- 100ml/kg i.e. 10x100 =1000ml
Second 10 kg- 50ml/kg i.e. 10 x50=
500ml
Rest of kgs- 20 ml/hr i.e. 5x 20= 100ml
Total =
1600ml for 24 hours
This maintenance fluid should be
added to the burn fluid requirement – say for example this 25 kg child had 25 percent
TBSA burn
i.e. using parkland formula
3x 25x 25
=1875ml add the maintenance 1600 ml
Total= 3475ml in 24 hrs
Divide by 2= 1738 ml in first 8 hrs
or divide this by 8= 217 ml each hr for the first 8 hrs
For the next sixteen hrs the fluid
will be 1738/16 i.e. 108ml per hour for the next sixteen hours.
This is only a calculation done as a
guideline and should not be rigidly adhered to. We at asktheburnsurgeon are comfortable with the modified parkland
formula and the fluid requirements as done above. We also add a small dose of
albumin or fresh frozen plasma from the second eight hours to help build up the
oncotic pressure that is lowered due to loss of plasma proteins.
Urine output in adult burn patients should
be around 0.5ml/kg/hr- 1ml/kg/hr
In children this should be around 1ml/kg/hr
Therefore a 25kg child should produce
at least 25 ml urine per hour
While in an adult of 50 kg a urine
output of 25-30ml would be just acceptable
The clinical parameters and the urine
output per hour should be kept in mind and the fluid requirement can be
increased or decreased to maintain all the clinical parameters in the normal
range. The monitoring should be done as in adults.
Children are more susceptible to burn
shock and therefore IV access should be rapidly obtained. Rarely an interosseus
live may be needed when these lines cannot be obtained. Glucose levels should
be frequently checked since hepatic glycogen levels are limited in children, and
addition of D5 Ringer lactate solution can help in preventing troublesome
hypoglycemia.
(An original initiative in burn
care and education from asktheburnsurgeon++)
Friday, April 11, 2014
SEVERE BURNS HAND - THUMB WITH CONTRACTURES...
Hello,
Dear Dr D W
Thanks you very much for your letter,
so sad to see this wonderful child suffer from this burn,
nice to hear your daughter is doing charity work abroad,
L...has a burn which is quite severe,
the burns must have been full thickness and would have needed a skin graft during the time of the burn episode ,
as no addition of tissue was done it healed secondarily causing very severe burn contractures,
My
daughter who is volunteering in Indonesia sent me a photo
yesterday of a little girl with a deformed thumb from an untreated burn
injury. She is asking if anything can be done for the child.
I have attached some pictures.
My
daughter writes, "L.. is a little over one year old and the
first burn incident happened when she was about 4 months and the second
incident happened when she was about 8 months (she rolled into the
fire.)"
Can you make a recommendation whether or not surgical intervention would be of benefit to her?
Thanks for you time,
Dr D W
Dear Dr D W
Thanks you very much for your letter,
so sad to see this wonderful child suffer from this burn,
nice to hear your daughter is doing charity work abroad,
L...has a burn which is quite severe,
the burns must have been full thickness and would have needed a skin graft during the time of the burn episode ,
as no addition of tissue was done it healed secondarily causing very severe burn contractures,
presently the contracture is severe as it appears,
its
has distorted the thumb joints and if untreated will end in severe
deformities in the future and she will be unable to effectively use the
thumb,
she needs surgery which will involve ,
releasing the thumb from its
present position and getting it back to its normal position,
once
done i think a large area of tissue defect will appear and this may
need a thick pad of tissue with skin ( flap cover as it is called in
plastic surgery ) rather than a thin skin graft,
choices of flaps include - radial artery flap, abdominal flap and free flap depending on the expertise available
sometimes if we are lucky we may be able to get away with a skin grafting procedure,(this can be made sure
of only at surgery),
we at asktheburnsurgeon hope that this sweet child can be helped somehow to regain back her function ....
with best regards
and wishes
asktheburnsurgeon++
Tuesday, April 8, 2014
Role of colloids in burn resuscitation...........
Doc, what is the role of albumin in
early burn resuscitation? Do we have to give it in all cases?
Jessie p,
Colorado, USA
When a patient suffers a burn injury
there is a temporary loss of the integrity of the capillaries as we have
discussed before. This loss leads to the leakage of plasma proteins like
albumin into the interstitial space. This
loss continues for the first eight hours following which the capillaries start
to regain their integrity. Therefore if one were to replace the colloids in the
first eight hours they would obviously leak out. It seems reasonable that one
may start to replace giving colloids in the 2nd eight hours of the burn.
Different types of colloids may be
used for resuscitation in burns: fresh frozen plasma, albumin and Dextran. Fresh
frozen plasma is often given at a rate of 0.5ml-1ml/kg %TBSA and has a
theoretical advantage - it replaces other plasma proteins besides albumin.
Dextran, another colloid used in burn
resuscitation increases capillary blood flow, reduces RBC aggregation and helps
to reduce tissue edema though this effect is limited to the time that Dextran
is being administered as the body will metabolize it eventually. Dextran is
composed of polymerized high molecular weight glucose chains and has double the
osmotic pressure of albumin.
Hypertonic saline (180-300 mEq/L) has
been used in some centers as it helps to shift extracellular fluids ( third
space fluid loss) back into the vascular space by osmosis resulting in a
reduction of fluid requirements. However there are some disadvantages:
hypernatremia and intracellular fluid depletion can occur and therefore serum
sodium levels should be closely monitored and maintained below 160mEq/L.
Albumin which is a regular component
of our plasma is a protein that maximally raises the intravascular oncotic
pressure. When it is given intravenously fifty percent of it remains intravascular,
when compared to other colloid solutions where only twenty to thirty percent
remains intravascular. Albumin is often infused as the rate of 0.3-1ml/kg /% burn
over 24 hours.
In many centers colloids are added in
the 2nd eight hours though Parkland formula advocates only crystalloids in the first 24
hours. Colloids help to reduce the fluid
load in the first 24 hours and they also help to increase the urine output
which often tends to go down during resuscitation. Colloid resuscitation is of
great benefit in geriatric patients, major burns (>40%), patients associated
with inhalation injury and those with cardiac disorders as it is difficult to
resuscitate them with limited fluids and they are constantly in the danger of
being overloaded. Fluid infusion should be tapered off after the first 24-32
hrs, when one finds that the patient has been adequately resuscitated. Fluid administration
should then be planned on the basis of requirements of albumin (keep>2) and
free water requirements (electrolyte free) to counter irreversible water loss. Free water
requirement is estimated as (25% + % burn) x BSA (m2) = ml/hr free water.
The maintenance of all the clinical parameters like the urine output at normal
levels is critical to the continuation of the resuscitation process to its
logical conclusion. Prudent use of fresh frozen plasma and albumin can be very helpful and safe when compared to other colloids in burn resuscitation.
(An original initiative in burn care and education from asktheburnsurgeon++)
Sunday, April 6, 2014
Monitoring the burn patient during burn resuscitation….
Doc, we recently had a patient with 80 percent burns. Though we
calculated the fluid loss and replaced it adequately the patient died. Could
you tell us why this may have happened?
Sohail k,
Karachi, Pakistan.
Patient with major burns have two
major issues that need to be dealt with:
a) Calculating the fluid requirement
and replacing it
b) Monitoring the burn patient to
know if the fluids replacements are adequate
We have already seen the calculation
of fluids requirements in a previous post. We shall have a look at how to
monitor burn patients. With fluid replacements there can be two issues-
inadequate fluid replacement or fluid overload. If the calculated fluids are
less then the patient will end up in shock and deteriorate. If the fluids are
over calculated then fluid overload, increased pulmonary complications and
increased compartmental pressure will result and finally end in circulatory
failure and collapse.
All burn patients must therefore be
monitored with great care. A number of
clinical parameters that are commonly used in ICU monitored patients are also
applicable here:
Pulse
Temperature
Respiration
Blood pressure
Oxygen saturation
Central venous pressure
Hourly urine output
These are the most common clinical
parameters used. As the body looses fluids from burns and the intravascular
pressure falls from the fluids shifts the blood pressure tends to fall. However
the human body has a lot of inbuilt mechanisms to control this fall and
deceptively maintains the blood pressure by releasing catecholamines or
chemicals which will cause contraction of the blood vessels and thereby
maintain the blood pressure. The pulse also rises from the pain reaction
(tachycardia). The body has a limit till which it can support the blood
pressure, once the fluid loss crosses this limit the homeostatic mechanisms
will fail and burn shock will result. The
increasing compartmental edema that results in burns can result in an erroneous
blood pressure reading. Similarly the vasospasm that occurs in the extremities
can lead to incorrect oxygen saturation reading by pulse oxymetry.
Urine output is one of the most
important parameters while monitoring the burn patient and this should be 0.5ml
(kg/hr) in adults and in children about
1ml (kg/hr). In most cases if an adequate urine output is maintained one can
assured of an adequate fluid resuscitation. Major burn patients will need
placement of a urinary catheter to monitor the hourly urine output. The volume
status can also be gained from the central venous pressure or CVP. Insertion of
a cvp line helps in monitoring this pressure and helps prevent fluid overload
in normal patients. However in patients with previous poor cardiac function or
in geriatric patients one may need the use of a swan ganz catheter. Similarly diabetic
patients and those using long term diuretics and also patients with
resuscitation difficulties may benefit from the use of the swan ganz catheter.
Pulmonary vasoconstriction may lead to faulty CVP or swan ganz measurements. Maintenance
of the acid base balance in the body as seen from the various blood gas
measurements and analysis suggest adequate resuscitation. Some patients with
cardiac co morbidities may need invasive cardiac monitoring. In these patients
one must be careful while increasing the fluid administered and should only be
done gradually to maintain adequate urine output (0.5ml/kg/hr adult and
1ml/kg/hr in children).
The requirement of fluid may be
higher than calculated in some patient groups. Those patients who have suffered
inhalation injury need 30-40%more fluids than suggested by Parkland formula. Patients with electrical
burns need more fluids as they have greater underlying tissue damage. Patients undergoing
diuretic therapy have prior free water deficits and need more fluids for
resuscitation. Patients who have undergone escharotomies and have large open
wounds may have higher free water losses that need to be adequately replaced. Patients
in whom resuscitation is delayed probably have higher inflammatory response, greater
fluid needs and attempts should be made to replace the fluid deficit calculated
by Parkland in the immediate resuscitation
period without causing hemodynamic failure.
(An original initiative in burn care and education from asktheburnsurgeon++)
Friday, April 4, 2014
Factors affecting the depth of the burn………
Doc, besides actually looking and evaluating the burn area is there other
ways of knowing that the burn area might be deep?
Marjorie A, Sidney, Australia
A
number of factors should be considered while evaluating the burn depth- temperature
at which the burn is caused, duration of contact, cause of burn and site of
burn.
The
area which is burnt is also important as the skin thickness varies at different
sites (from 1 mm in the genitalia and eyelids to 5 mm in palms and soles). The skin is relatively thinner in children and
geriatric patients and therefore they tend to suffer a greater degree of burns.
Contact
burns tend to be deeper since the burning object or the hot object like the exhaust
of a motorcycle remains in direct contact and causes more damage to the skin.
It must be noted that the lesser the duration
of the burn, the lesser the degree of burn. Therefore it is recommended that
the burn area be cooled at the earliest. Pouring cold water over burns areas
works on this principle and one must within seconds carry out this maneuver to
avoid severe burns. The home kitchen is one area where burns often occur. Fortunately
water is always available in the kitchen and therefore quickly pouring cold or
tap water over the burn area works wonders and one should let the cold water
run over the burn area for a few minutes.
Application
of oil or mint preparations as is often done by lay people should be avoided as
oil stops the heat loss from the surface causing more damage and mint just
gives cools the mind and not the burn area.
The
cause of the burn should be inquired into as different modes of burns can cause
different depths of burns. For e.g. hot water burns are less deep than hot frying
pan oils, as the temperatures of hot oil touch 175-200 degrees compared to hot
water which may be 75-100 degrees. Different acids and bases can cause
different degree of burns depending on their strengths. Thus knowing the burn agent helps a lot in deciding the depth of the burn and predicting the outcome.
We shall discuss how the monitor burn patients in our next post....
(An original initiative in burn care and education from asktheburnsurgeon++)
Thursday, April 3, 2014
Resuscitation Fluids and formulae……….
Doc, how much fluids should be given to a burn patient and
can a person survive if fluids are given if the patient comes to the hospital
many hours after the burn incident?
Shawn, California
As we discussed in an earlier
post, burn wounds loose body fluids from the wound surface as the skin
integrity is damaged. Greater the surface area of the burn, more the fluid
loss. In general the body is able to tackle the fluid loss that occurs from a
less than 15 percent TBSA (total burn surface area) in an adult, and less than 10 percent TBSA in a
child. Beyond this the body’s internal mechanisms are unable to handle this
loss and the patient will end up in shock if the lost body fluids are not
replaced. Once we understand this concept then we are faced with two questions:
a) At what rate should we
administer the intravenous fluids?
b) What is the type of
fluid that we should administer?
Parkland formula
Charles Baxter from parkland hospital
(Texas, USA) made a large contribution to the management
of burns by his studies on the fluid loss in burns and their replacement. He observed
that the first 24 hours were critical to the survival of burn patients and the replacement
of fluids was to be done in the first 24 hours itself. In this the first 8
hours were crucial as the blood vessels and capillaries lost their integrity
totally and therefore the intravascular fluids leaked out on a large scale. In the
second 8 hours after the burn the capillaries regained their integrity and the
leaks were controlled to a great extent. Keeping this in mind Charles Baxter suggested
a fluid resuscitation formula in burn patients at 4 ml/kg/TBSA for the first 24
hours. The type of fluid suggested was Ringer Lactate. Of the total fluid calculated for 24 hours,
half of the volume was to be given in the first 8 hours and the rest in the
next sixteen hours.
Why did Baxter suggest Ringer Lactate
as the resuscitation fluid?
Obviously because he observed that it was more
physiological and had many advantages:
a) Ringer lactate has a lower sodium
concentration (130mEq/L) than normal saline. b)The metabolized lactate had a buffering effect on associated metabolic acidosis in burns.
c)Ringer lactate is an Isotonic crystalloid solution
Example for fluid calculation:
Let’s take an example here – a patient
with a body weight of 65 kg comes to the
ER with flame burns of 45 percent TBSA.
TBSA 45%
Weight of the patient- 65 kg
Therefore the fluid calculation by
parkland formula-
4x% TBSA x body weight
i.e. 4 x 45 x 65
i.e. 11,700 ml for 24 hours
Half of this has to be given in the
first 8 hours
i.e. half of 11,700 – which is 5850
ml for 8 hours
Therefore for each hour in the first
8 hours the patient needs 5850/8 ie 731.25 ml or approximately 730ml per hour
For the next 16 hours the remaining
11700 ml needs to be spread out
So 5850/16 is 365 ml needs to be
given each hour for the next 16 hours
Thus the patient must receive 730 ml
per hour for the first 8 hours post burn and for the remaining 16 hours of the
first day the patient must receive 365 ml per hour.
Coming to the second part of the question- the fluid calculated has to be replaced in the time specified. However some patients appear later than the time of the burn and therefore the fluids which were not administered will have to be replaced at a higher rate but taking care to see that we do not overload the patient and put him into cardiac failure or pulmonary edema.
It must be noted that the calculation
of fluids by this formula is only a guide line and a number of factors must be
taken into consideration which administering fluids which we shall discuss in
another post …..
(An original initiative in burn care and education from asktheburnsurgeon++)
Wednesday, April 2, 2014
Classification of burns...........
Doc, are there different ways to
classify burns?
Mrs. Janice Parker. S. Africa.
Yes there are different ways to
classify burns, but the whole purpose is to help in managing them in a better
way. Every burn must be mentioned by its
degree or depth since it lets the surgeon know whether he should manage the
patient conservatively or by surgery. Further classifying burns in major, minor
or moderate helps to decide the level of management that they need. Thus a
third degree burn even if it is one percent TBSA (total burn surface area) cannot be managed
conservatively and will need surgery. Again a 5 percent TBSA can be managed on
an outpatient basis, but a 50 percent TBSA will definitely need inpatient
management.
degree of burns.
Degree of burn
actually tells us about the depth of the burn. The burn depth is classified as
follows.
a) First degree- superficial
burns affecting the epidermis are referred to as first degree burns and are
similar to sunburns.
b) Second degree: both the epidermis and the
superficial layer of the dermis are damaged in second degree burns.
c) Third degree
burns: these burns affect the full thickness skin and often needs surgical
management.
d) Fourth degree
burns: these burns affect the full thickness of the skin and the underlying
structures like nerves, muscles, tendons, vessels and may extend up to the
bone.
We can also classify burns according
to their size:
a)Major Burns: these consist of chemical or high voltage electrical burns, Inhalation
injury, full thickness burns more than 10% TBSA or burns involving more than
25%TBSA.
b) Moderate Burns: these consist of Superficial
or partial thickness burns of trunk, hands, feet, perineum or head involving
15-25% TBSA.
c) Minor Burns: these
consist of Burns not involving the hand, perineum,
feet or head and must be less than 15% TBSA.
(An original initiative in burn care and education from
asktheburnsurgeon+)
Tuesday, April 1, 2014
ASSESSMENT OF BURN SURFACE AREA……
Doc, what happens if I calculate the burn area wrongly? Is it
really important?
Arthur A, Canada
As we have seen in
previous posts the loss of fluid from the skin surface depends on the degree of
burns and the area of the burns. One must evaluate the total burn surface area
(TBSA) to calculate the fluid requirements. There are different methods of
fluid calculation in burns.
a) Rule of nine
The rule of nine works
well in adult patients. In this method the body surface is divided into various
parts measuring in nines.
Rule of nine
Each arm - 9% TBSA
Head - 9% TBSA
Anterior thorax - 18%
TBSA
Posterior thorax - 18%
TBSA
Perineum - 1% TBSA
Each leg - 18% TBSA
Any burn surgeon will tell you that more
often the burns are so irregularly placed that accurate calculation becomes
difficult in different regions of the body. In such cases a simple trick is to
use the palm of the hand as a method of calculation. At any age the palm of the
hand is approximately 1% and can be used to measure the burn areas. One must not forget that it is the patient’s
hand that is used for the calculation and not the doctor’s. An approximate size
of the palm of the patient is considered and the equivalent burn area is
estimated. For e.g. lets say the burn area was 5 palm sizes of the patient over
the body and lower limbs. Now we can assume that the patient has about 5% burns.
It should be noted that first degree
burns do not produce fluid losses and therefore only 2nd degree
burns or more should be used for fluid calculation.
However in children the rule of nine
can lead to serious errors as the head and body is larger in TBSA than the
limbs and therefore the Lund and Browder charts work out to be
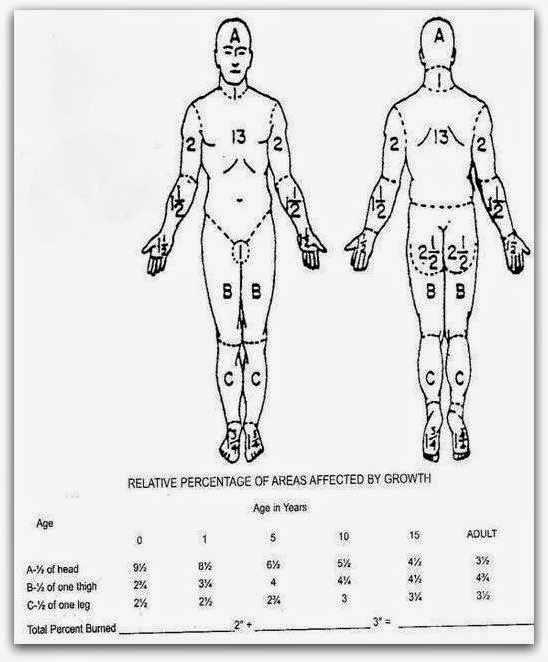
more accurate while calculating the fluids to be administered. The Lund and Browder chart is shown below.
If the fluid calculation is wrong
then the patient will be administered less fluids and this will result in shock
or low volume circulatory failure and ultimately may be fatal. The fluids calculated need to be replaced
within a time limit as we shall discuss in the next post. Correct volume replacement
and correct timing is what makes the resuscitation of burns patients
successful.
(an original initiative in burn care and education from
asktheburnsurgeon+)
Sunday, March 30, 2014
How burns affect the tissues.....
Doc, could you please explain the cellular and chemical
processes that occur when the tissues are burnt?
Rony v, Goa
A number of inflammatory processes both local (at the site of
the burn) as well as systemic (in the rest of the body) take place when burns
occur which eventually lead to the shifting of fluid from the vascular
compartment to the interstitial spaces. Subsequent to the burn a number of
cells like Neutrophils,
macrophages, and lymphocytes cross over into the burned tissues and start releasing
chemical mediators like histamine, serotonin, prostaglandins, kinins, platelet
products and complement components. These chemical substances damage the normal
blood capillary barrier which leads to an increase in the permeability of the
vessels. Intravascular fluids therefore start to leak from the walls of the
vessels and this ultimately leads to a decrease of the circulating
intravascular blood volume. A fact that is not commonly recognized is that
these processes that occur in the burn tissues also take place in the tissues
that have not suffered any burns and therefore one can see edema in areas of
the body that have not suffered burns. Thermal injury also ends up damaging the
cell wall and collagen fibers which in turn lead to inadequacy of the cell wall
transport mechanisms and buildup of sodium and water and eventual death of the
cell if the fluid imbalances are not immediately corrected. In minor burns such
as 10 percent in children and about 15 percent in adults these fluid balances
are well adjusted and tolerated and therefore additional fluid replacements are
not needed. However in patients with TBSA higher than the one’s mentioned above
intravenous fluid resuscitation is needed.
The capillaries begin to
regain their functional integrity and the leak eventually gets controlled, but
this often takes more than 8 hours post burn. Crystalloids are usually given in
the first 8 hours and one’s the integrity of the capillary wall is regained
after 8 hours, colloid fluids are started since they will not leak out. Adding
colloids also help to reduce the fluid overload that may result of excess of
crystalloid infusions. Burn wounds are composed of three zones- a central zone
of coagulation or severe tissue damage, a peripheral zone of hyperemia or
vasodilatation, and an intervening zone
of stasis or low blood flow (ischaemia). If the fluid imbalances that occur
from the fluid shifts as noted above are not corrected on time then these zones
can extend and more tissue damage can result explaining the fact that some
superficial burns on admission can end up as deep over period of time. This can
also happen when burn wounds get infected.
(an original initiative in burn care education from asktheburnsurgeon)
+
Monday, March 24, 2014
Burns, fluid therapy, burn management, fluid resuscitation in burns
Doc why is
fluid therapy so important in burn patients?
Neeraj,
Pune, India
Till the nineteenth
century burn patients had a high mortality rate. Why so many patients died in
the early stage of burn treatment remained a mystery till the concept of body
fluids in different compartments became clear. The body fluids lie in three
different compartments- vascular (within the blood vessels), intracellular (within
the cells) and extracellular space (outside the cells and blood vessels). A
constant shift of fluids keeps occurring to maintain a balance between these
three spaces and they remain in a state of equilibrium.
Among the organs of the
body the skin is the largest – about 15% of body weight and roughly 1.7 sq meter
in surface area. While the skin has a large number of functions like sensation,
physical protection, temperature regulation and others, the function of prevention
of fluid loss is critical to the burn management. Skin is made up of two
critical components –dermis and epidermis. Burns damage the integrity of the skin and
destroy its ability to manage fluids effectively. A lot of chemical substances
are released due to the burn injury which increases the leaking of fluids from
the vascular compartment to the extracellular space causing edema or tissue
swelling. This edema may be insignificant in small burns but in large burns or
burns more than 10 percent in children and 15 percent in adults can lead to loss of
water, albumin, sodium and red blood cells which can lead to a sudden fall in
the vascular space compartment pressure and shock (burn shock)- culminating in
death if not properly treated. The larger the TBSA of burn (Total body surface area) the greater the risk of death. The fluid loss need to be calculated correctly
and has to be replaced. Some historic events like the coconut groove fires and
other mass casualties led researches to understand the importance of fluid
management especially in the initial stage of burn management.
It is believed that every
year, 2.5 million Americans sustain a significant burn injury of which about 100,000
are hospitalized, and around 10,000 die. Burn researchers - Underhill and Moore
were the first to identify the concept of thermal injury- induced intravascular
fluid deficits in the early nineteenth century, followed by Evans who
introduced the fluid resuscitation formula in 1952. More than 50 percent of
patients with 50% TBSA or more died in the past and
now this mortality has come down to less than 10 percent – all because of the clear
understanding of fluid management in burn care.
(An original initiative in burn care education from asktheburnsurgeon!!!)
+
Subscribe to:
Comments (Atom)